Most people don’t give much thought to their tonsils. Hidden in the back of the throat, these tiny organs are out of sight and out of mind. Often, it isn’t until something goes wrong with their tonsils that people pay them much mind. They were even once thought to be vestigial structures. Tonsils, however, are more than meets the eye. In this article, we will review the tonsils’ function and anatomy, relevant health conditions, and more.
Purpose and Function
Tonsils are a group of tissues that serve as the body’s first line of defense against pathogens entering through the nasopharynx and oropharynx, which are tubes that connect your nose and mouth to your throat.1 This collection of tissue is known as mucosa-associated lymphoid tissue (MALT). MALT has a specific and important role in helping the body fight infection. Its primary function is to participate in the secondary immune system by sampling antigens and local pathogens that enter the mouth and nose and stimulate further immune response.2
Anatomy of the Tonsils
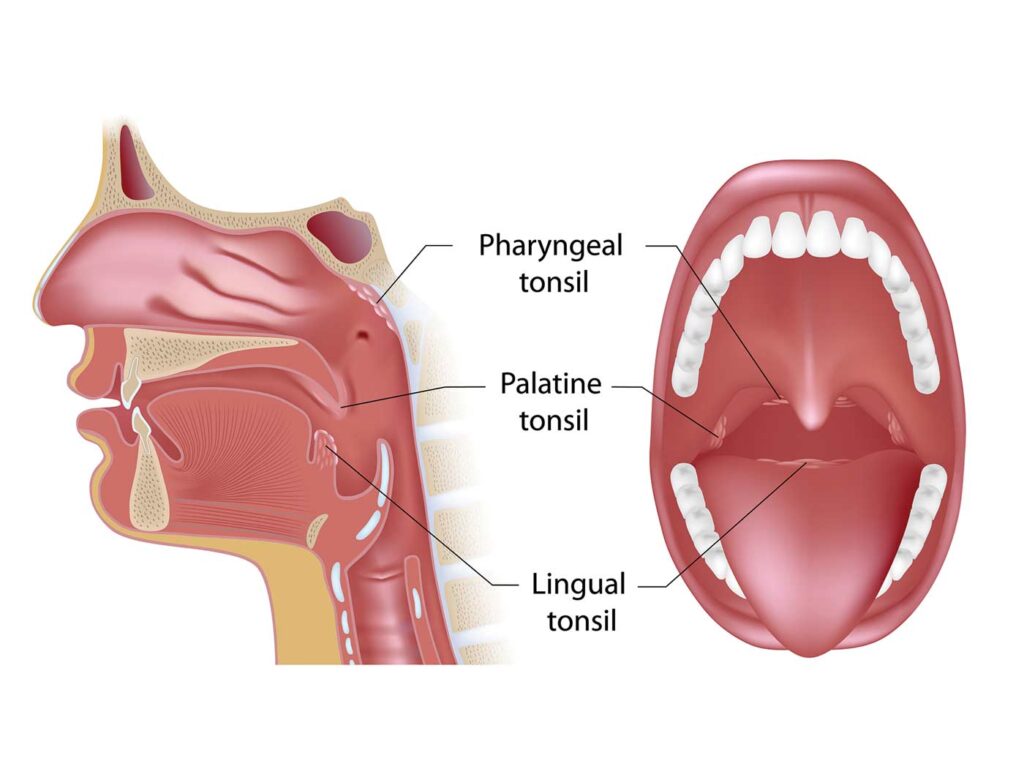
The body has four different types of tonsils all located in the pharynx, which is the upper part of your throat located behind your nose and mouth.3 Most people are familiar with the palatine tonsils. This fleshy, oval-shaped pair sits far in the back of the throat on either side of the uvula. It is the only set you can see without assistance.4,5 The pharyngeal tonsil, a single tonsil also known as the adenoid, is located in the nasopharynx above and behind the soft palette. The third set of tonsils, which are located at the base of the tongue, are the body lingual tonsils. Finally, tubal tonsils are set in the nasopharynx wall near the opening to our eustachian tubes, which connect the middle ear with the nasal-sinus cavity.1 Together, these tonsils form a circular band at the back of the throat called Waldeyer’s ring. Their unique ringed arrangement allows them to effectively guard the entrance to the digestive and respiratory systems, two of the body’s most important systems that interact with the outside world.5–7
Healthy palatine tonsils are pink or red in color and don’t take up much room in the throat.4 While their size might vary slightly across the general population, most end up being about the size of a lima bean in adulthood.1,3,8 One characteristic that does not change across the lifespan is their irregular surface. Some people might be surprised to find that ridges and small “holes” called crypts line their tonsils. These folds are typical and naturally occurring. However, it is this anatomical structure, as well as their role in the immune system, that makes the palatine tonsils and adenoid susceptible to infection.
Health Conditions: Definition, Risk Factors, Cause(s), and Symptoms
Redness and inflammation are two trademark signs that the palatine tonsils are infected by a virus or bacteria.1,3,5–8 Sometimes, adenoids become infected and swell simultaneously. These symptoms can cause significant pain and even obstruct breathing and swallowing. While several conditions can affect this organ, tonsillitis, tonsil stones, and peritonsillar abscesses are the most common.
Tonsillitis. Tonsillitis is a generic term that describes swelling of the palatine tonsils.6–11 It is the most common condition affecting these organs and is more common among children than adults.3,5,10 About 70 percent of these cases are caused by viruses, such as the flu and the common cold, but bacterial infections can also cause the tonsils to swell.1,9 Inflammation and redness are the most common signs of tonsillitis, but other symptoms, including throat and ear pain, swollen glands, fever, bad breath, chills, and a white or yellow coating on your tonsils, can also be present.11,12 These cases fall into three categories: acute (isolated cases where symptoms last between 3–14 days), recurrent (multiple cases per year), and chronic (cases where symptoms last more than 14 days).1,3,9–14 Treatment for tonsillitis often depends on the severity of frequency of infection. Most cases can be treated at home with salt water or medicated gargles, over-the-counter pain medicine, increasing indoor humidity, and drinking warm liquids.15 A doctor will only prescribe antibiotics when tonsillitis is caused by a bacterial infection, such as strep throat.
Tonsil stones. Tonsil stones, or tonsilloliths, are small white or yellow pebble-like lumps that appear on the surface of palatine tonsils. These deposits are typically unilateral, appearing on either the left or right tonsil, and are made up of bacteria, food debris, and minerals, like calcium, that harden and lodge in the ridges and crypts.13–16 Tonsilloliths are relatively common, with most cases occurring in adulthood and people with recurrent tonsillitis.17 Cases are usually innocuous and sometimes asymptomatic. However, their side effects can be a nuisance. The most common symptom is bad breath, but some people also develop a cough, sore throat, or difficulty swallowing.14,15,18 As with tonsillitis, removing tonsil stones usually does not require visiting a doctor. Some studies suggest gargling salt water or manually dislodging them with a water flosser, but most cases resolve over time without intervention.13,14 Larger or recurrent stones, however, may require removal by an otolaryngologist, a healthcare provider who specializes in ear, nose, and throat disorders.
Peritonsillar abscess. Also known as quinsy, peritonsillar abscess (PTA) is a bacterial infection that causes pus to collect next to the tonsils in the back of the throat.1,3,19–22 It is often a complication of tonsillitis. PTA is the most common deep head and neck infection in the United States (US); a 2023 study estimates an incidence of approximately 1 in 10,000, with most cases occurring in young adults.21,23,24 Symptoms include severe pain and swelling on one side of the throat, roof of the mouth, or neck; difficulty swallowing; fever; drooling; and red, inflamed tonsils.19–23 PTA requires immediate attention. If caught early enough, the abscess can be treated with antibiotics.20 The pus-filled pocket can swell enough to shift the uvula and even obstruct the throat without immediate treatment. Preventing the PTA from rupturing is crucial because the pus can spread the infection throughout the body. An otolaryngologist will treat the abscess by draining it and carefully removing the fluid.20,24,25 Recovery from this procedure lasts from 4 to 6 days, but an estimated 10 percent of PTA infections will recur.22,26
When it comes to keeping your tonsils healthy, prevention is the best medicine. Good oral hygiene—brushing your teeth and tongue, flossing regularly, and rinsing your mouth after meals—not smoking, and staying hydrated can all help prevent these conditions from developing.3,7,13,14 However, there is no surefire way to prevent tonsil infections. Some people are simply more prone to them.1,3,27,28 In these cases, a tonsillectomy and adenoidectomy, procedures that remove these tonsils altogether, might be necessary.
Surgical Options
In addition to the conditions mentioned above, tonsillectomies and adenoidectomies may be performed on people who have enlarged tonsils, which are a major risk factor for obstructed and sleep-disordered breathing.1,3,28 These procedures are some of the most common surgical operations in the US. In fact, tonsillectomies and adenoidectomies, often abbreviated as T&A, were the most frequently performed procedures in the US between 1915 and the mid-1960s.30 While this rate has declined, more than 500,000 tonsillectomies are performed annually in children less than 15 years of age.31,32
Patients are under general anesthesia during these surgeries. Tonsillectomies and adenoidectomies, which usually happen at the same time, typically last between 30 to 60 minutes when performed together.32–34 Surgeons may use a scalpel, surgical snare, laser, or cauterization to remove the tonsils. Once the operation is complete, the patient will be moved into a recovery area where their care team will check their vitals and monitor their status. While these surgeries can be outpatient procedures, some doctors may require tonsillectomy and adenoidectomy patients to spend the night in the hospital to rule out postoperative complications.
The amount of time it takes to recover from these procedures depends on several factors, including the health and age of the patient, the extraction method used, and how closely recovery instructions are followed.35,36 Common post-procedure symptoms include nausea, lack of appetite, general fatigue, and soreness in the throat, ears, neck, and jaw. A full recovery can take up to two weeks, with younger children often bouncing back after several days. At any age, there’s an increased risk of bleeding after surgery, particularly within the following 7 to 10 days.3,5,33,35 Given this, all tonsillectomy and adenoidectomy patients should rest during this period and consider using over-the-counter painkillers to relieve swelling and discomfort.
Bottom Line
While their purpose and function are often under appreciated, your tonsils—all four types—play a critical role in staying healthy. Their ability to filter through and fight pathogens helps protect your body from infection. Though their ringed arrangement at the top of the throat uniquely positions them to fight disease, it also makes them more susceptible to certain health conditions. Luckily, proper preventative care and consistent oral hygiene can keep your tonsils healthy and functional.
Sources
- Arambula A, Brown JR, Neff L. Anatomy and physiology of the palatine tonsils, adenoids, and lingual tonsils. World J Otorhinolaryngol Head Neck Surg. 2021;7(3):155–160.
- Elmore SA. Enhanced histopathology of mucosa-associated lymphoid tissue. Toxicol Pathol. 2006;34(5):687–696.
- Welsh E, Allman-Updyke E. Ep 134 Tonsils: underestimated and underappreciated. This Podcast Will Kill You. 30 Jan 2024. http://thispodcastwillkillyou.com/wp-content/uploads/2024/02/TPWKY-Episode-134-Tonsils.pdf. Accessed 1 Mar 2024.
- Holland K. How to examine your tonsils. Healthline. 26 Sep 2023. https://www.healthline.com/health/how-to-examine-your-tonsils. Accessed 17 Mar 2024.
- American Academy of Otolaryngology–Head and Neck Surgery Foundation. Tonsils and adenoids. 1 Feb 2019. https://www.enthealth.org/conditions/tonsils-and-adenoids/. Accessed 11 Mar 2024.
- Vang P. Tonsils: tiny, but pack a big punch. Mayo Clinic. 13 Apr 2023. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/tonsils-tiny-but-pack-a-big-punch. Accessed 18 Mar 2024.
- Anderson J, Paterek E. Tonsillitis. In: StatPearls. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK544342/.
- Cheriyedath S. Functions of tonsils. Medical Live Science. 25 Oct 2018. https://www.news-medical.net/health/Functions-of-Tonsils.aspx. Accessed 18 Mar 2024.
- Mayo Clinic Staff. Tonsillitis. Mayo Clinic. 3 Sep 2022. https://www.mayoclinic.org/diseases-conditions/tonsillitis/symptoms-causes/syc-20378479. Accessed 16 Mar 2024.
- Morales-Brown P. All you need to know about tonsillitis. Medical News Today. 26 Jun 2023. https://www.medicalnewstoday.com/articles/156497. Accessed 20 Mar 2024.
- Carolina Ear Nose & Throat – Sinus and Allergy Center. 7 amazing facts about your tonsils. 7 Jul 2019. https://carolinaearnosethroat.com/7-amazing-facts-about-your-tonsils/. Accessed 2 Mar 2024.
- Kaneshiro N. Tonsillitis. Penn Medicine. 31 Oct 2022. https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/tonsillitis. Accessed 20 Mar 2024.
- Abu Bakar M, McKimm J, Haque SZ, et al. Chronic tonsillitis and biofilms: a brief overview of treatment modalities. J Inflamm Res. 2018;11:329–337.
- Yellamma Bai K, Vinod Kumar B. Tonsillolith: a polymicrobial biofilm. Med J Armed Forces India. 2015;71(Suppl 1):S95–S98.
- Bathala S, Eccles R. A review on the mechanism of sore throat in tonsillitis. J Laryngol Otol. 2013;127(3):227–232.
- Cleveland Clinic. Tonsil stones. 7 Jan 2024. https://my.clevelandclinic.org/health/diseases/21505-tonsil-stones. Accessed 25 Mar 2024.
- Bamgbose BO, Ruprecht A, Hellstein J, et al. The prevalence of tonsilloliths and other soft tissue calcifications in patients attending oral and maxillofacial radiology clinic of the University of Iowa. ISRN Dent. 2014;2014:839635.
- Aylıkcı BU, Colak H. Halitosis: from diagnosis to management. J Nat Sci Biol Med. 2013;4(1):14–23.
- Hayes K. An overview of peritonsillar abscess. Verywell Health. 30 Aug 2022. https://www.verywellhealth.com/peritonsillar-abscess-3958291. Accessed 23 Mar 2024.
- MedlinePlus. Peritonsillar abscess. 29 Nov 2022. https://medlineplus.gov/ency/article/000986.htm. Accessed 24 Mar 2024.
- Gupta G, McDowell RH. Peritonsillar abscess. In: StatPearls. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK519520/
- Galioto NJ. Peritonsillar abscess. Am Fam Physician. 2017;95(8):501-506.
- Cleveland Clinic. Peritonsillar abscess. 18 Apr 2022. https://my.clevelandclinic.org/health/diseases/22817-peritonsillar-abscess-quinsy. Accessed 18 Mar 2024.
- Klug TE. Peritonsillar abscess: clinical aspects of microbiology, risk factors, and the association with parapharyngeal abscess. Dan Med J. 2017;64(3):B5333.
- Klug TE, Greve T, Hentze M. Complications of peritonsillar abscess. Ann Clin Microbiol Antimicrob. 2020;19(1):32.
- Chung JH, Lee YC, Shin SY, Eun YG. Risk factors for recurrence of peritonsillar abscess. J Laryngol Otol. 2014;128(12):1084–1088.
- Cleveland Clinic. Tonsils. 8 Jul 2022. https://my.clevelandclinic.org/health/body/23459-tonsils. Accessed 26 Mar 2024.
- National Institutes of Health.Understanding recurrent tonsillitis. 26 Feb 2019. https://www.nih.gov/news-events/nih-research-matters/understanding-recurrent-tonsillitis. Accessed 11 Mar 2024.
- Mayo Clinic Staff. Tonsillectomy. Mayo Clinic. 3 Sep 2022. https://www.mayoclinic.org/tests-procedures/tonsillectomy/about/pac-20395141. Accessed 26 Mar 2024.
- Grob GN. The rise and decline of tonsillectomy in twentieth-century America. J Hist Med Allied Sci. 2007;62(4):383–421.
- Cleveland Clinic. Tonsillectomy. 17 Oct 2022. https://my.clevelandclinic.org/health/treatments/15605-tonsillectomy. Accessed 25 Mar 2024.
- Bohr C, Shermetaro C. Tonsillectomy and adenoidectomy. In: StatPearls. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK536942/.
- Weill Cornell Medicine. What parents should know about tonsillectomy and adenoidectomy. 18 Feb 2021. https://weillcornell.org/news/what-parents-should-know-about-tonsillectomy-and-adenoidectomy. Accessed 26 Mar 2024.
- Lambert EM, You P, Kacmarynski DS, Rosenberg TL. Adenoidectomy and persistent velopharyngeal insufficiency: considerations, risk factors, and treatment. Int J Pediatr Otorhinolaryngol. 2021;149:110846.
- Hayes K. How long does it take to recover from a tonsillectomy? Very Well Health. 13 Oct 2022. https://www.verywellhealth.com/how-long-does-it-take-to-recover-from-a-tonsillectomy-1192159. Accessed 26 Mar 2024.
- Verma R, Verma RR, Verma RR. Tonsillectomy-comparative study of various techniques and changing trend. Indian J Otolaryngol Head Neck Surg. 2017;69(4):549–558.





