 According to the American Cancer Society, of the 13,400 annual cases of cervical cancer, 4,290 patients (>33%) will die from the disease. This high mortality rate is due to the symptomatic complexity of cervical cancer, which can allow the cancer to spread and worsen before a diagnosis is made and treatment administered. In an effort to reduce mortality and improve outcomes of those diagnosed with cervical cancer and to prevent /reduce the occurrence of cervical cancer through public education, the United States Congress designated January as Cervical Cancer Awareness Month.
According to the American Cancer Society, of the 13,400 annual cases of cervical cancer, 4,290 patients (>33%) will die from the disease. This high mortality rate is due to the symptomatic complexity of cervical cancer, which can allow the cancer to spread and worsen before a diagnosis is made and treatment administered. In an effort to reduce mortality and improve outcomes of those diagnosed with cervical cancer and to prevent /reduce the occurrence of cervical cancer through public education, the United States Congress designated January as Cervical Cancer Awareness Month.
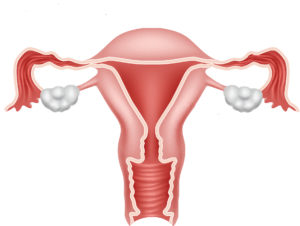
Functions of the Cervix
The cervix is a part of the female anatomy that connects the vagina to the uterus. Though it accounts for the lower third of the entire uterus, the length of the cervix tends to vary with age, childbirth, and genetics; typically, the cervix is around 2 to 4 centimeters long and is a tubular shape.However, its shape and color can change throughout the menstrual cycle. Compared with other uterine tissue, the cervix is more densely fibrous and rigid.3
Within the sturdy tissue lies a mucus membrane and cells that secrete fluids.3 These fluids serve many functions, such as moving sperm toward the egg(s) during ovulation and keeping harmful elements from entering the body. Conversely, when the female reproductive system is not ovulating, any mucus/fluids produced by the cervical membrane will become thicker, creating a barrier so sperm are unable to enter the uterus. To boot, a type of enzyme, known as lysozyme, found in cervical mucus can combat particular bacteria and protect against infection.3 During pregnancy, the cervix helps to station the baby in place until it’s fully developed, widening during childbirth to allow passage of the infant.3
Cervical Diseases and Their Risk Factors
Although the cervix is composed of sturdy matter, it can still develop health problems, such as inflammation caused by infection, polyps, dysplasia, and cancer.
Inflammation. When the cervix becomes inflamed, this is called cervicitis.4 Though cervicitis can be caused by noninfectious factors (e.g., allergic reaction, radiation/chemo, malignancy, local trauma, bacterial overgrowth of bacteria normally present in the vagina), it is most often the result of a sexually transmitted infection, such as chlamydia or gonorrhea. Those with cervicitis might experience an influx of vaginal discharge, painful and frequent urination, pain during intercourse or pelvic exam, and/or bleeding after intercourse or between periods. However, cervicitis does not often prompt any signs or symptoms; thus, many individuals are not aware they have the condition until undergoing a routine pelvic exam. The greatest risk factors for cervicitis include high-risk sexual behavior (e.g., unprotected sex, sex with multiple partners, sex with a person who engages in high-risk behavior); engaging in sexual intercourse at an early age; and/or history of sexually transmitted infections.4
Polyps. While the cause of polyps (bulbous growths) is not fully understood, their development in the cervix has been correlated to cervical inflammation and atypical hormone responses.5 Those with a cervix who are over the age of 20 and who have had at least one child are at higher risk of developing polyps.5 The two types of cervical polyps include ectocervical, which form on the outer layers of cervical cells and are more common in postmenopausal individuals, and endocervical, which form in cervical glands and are more common in premenopausal individuals. Bleeding between periods, heavier flow during menstruation, bleeding after intercourse, and foul-smelling discharge are symptoms of both polyp types. Though, like cervicitis, cervical polyps might not elicit any noticeable symptoms.
Dysplasia. Cervical dysplasia (abnormal cell and tissue) is a precancerous condition caused by the human papillomavirus (HPV), a sexually transmitted viral infection. Annually, cervical dysplasia affects 250,000 to 1,000,000 biologically female individuals in the United States. Those at greatest risk of developing cervical dysplasia are between the ages of 25 and 35 years of age who are sexually active. If not managed, cervical dysplasia can develop into malignant cancer.
Smoking, exposure to second-hand smoke exposure, having multiple sexual partners (though HPV can also be contracted through just one sexual partner), older age, skipping annual pelvic examinations, and being immunocompromised can increase the risk for cervical cancer.6 Those in the early stages of cervical cancer, when the cervical dysplasia becomes cancerous and permeates the surrounding tissue, typically do not exhibit symptoms. However, some might experience painful intercourse, heavier postmenopausal bleeding, heavier bleeding during menstruation, and bleeding during and after sexual intercourse and pelvic exams.7
Preventative Measures
Due to the asymptomatic and overlapping nature of the above conditions, especially during the early stages of cancer, annual pelvic examinations and Papanicolaou smear (pap) tests performed by a qualified healthcare provider are integral for cervical health and cancer prevention/management. The protocol for a pap test/pelvic exam consists of a doctor “gently scraping” the surface of the cervix using a small spatula and a small brush or cotton swab to gather cervical cells, which are examined under a microscope for signs of abnormalit8 Pap tests can detect abnormal cell before cancer develops. Indeed, cases of cervical cancer have decreased over the last 40 years due to increased preventative testing. During an annual pelvic exam, patients can also be tested for the HPV. Pap smear tests are recommended for biologically female individuals who are sexually active, smoke, have multiple partners, and/or have a history of infection with certain strains of HPV.8
In addition to regular pelvic examinations, following up with your physician if you receive abnormal pap test results, practicing safe sex, and quitting smoking are the best methods to prevent or manage precancerous changes of the cervix that can develop into cancer and other related conditions.9
Sources
- American Cancer Society site. Key statistics for cervical cancer. Updated 12 Jan 2021. https://www.cancer.org/cancer/cervical-cancer/about/key-statistics.html. Accessed 12 Jan 2021.
- National Cervical Cancer Coalition site. Cervical health awareness month. https://www.nccc-online.org/hpvcervical-cancer/cervical-health-awareness-month/. Accessed 12 Jan 2021.
- Encyclopaedia Britannica site. Cervix. Updated 28 Mar 2019. https://www.britannica.com/science/cervix. Accessed 12 Jan 2021
- Mayo Clinic site. Cervicitis. Diseases and conditions. https://www.mayoclinic.org/diseases-conditions/cervicitis/symptoms-causes/syc-20370814. Accessed 12 Jan 2021.
- Harvard Health Publishing site. Cervical polyps. Feb 2019. https://www.health.harvard.edu/a_to_z/cervical-polyps-a-to-z. Accessed 12 Jan 2021.
- Johns Hopkins Medicine site. Cervical dysplasia. Sidney Kimmel Cancer Center: cancers we treat. https://www.hopkinsmedicine.org/kimmel_cancer_center/cancers_we_treat/cervical_dysplasia/about_cervical_dysplasia/. Accessed 12 Jan 2021.
- New York State Department of Health site. Frequently asked questions about cervical cancer. Updated Oct 2018. https://www.health.ny.gov/diseases/cancer/cervical/faq/.
Accessed 12 Jan 2021. - Harvard Health Publishing site. Pap Test (Papanicolaou Smear). Dec 2019. https://www.health.harvard.edu/womens-health/pap-test-papanicolaou-smear. Accessed 12 Jan 2021. Rush University Medical Center site. Preventing Cervical Cancer. 27 Jun 2014. https://www.rush.edu/news/preventing-cervical-cancer.
Accessed 12 Jan




