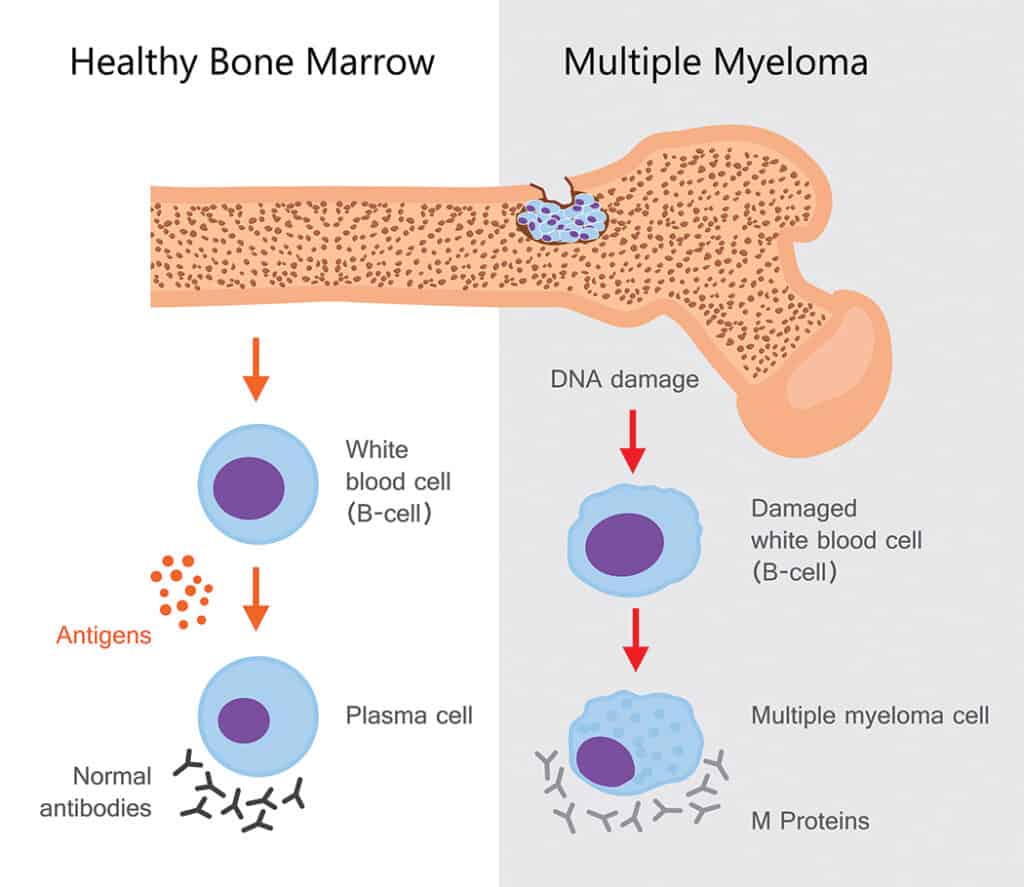
Multiple myeloma (MM) is a complex hematologic malignancy (blood cancer) characterized by the proliferation of malignant plasma cells and abnormal production of monoclonal antibodies (M protein). Overproduction of these plasma cells can cause end-organ damage.1 These plasma cells are found in the bone marrow.2 The cause of MM is unknown, but some risk factors have been identified. MM develops primarily in older adults, with the median age at diagnosis being 70 years. Men are 1.4-times more likely to have MM than women.1 MM risk is twice as high in Black/African American individuals, compared to White individuals, whereas Asian/Pacific Islander individuals have a lower risk. Additionally, Black/African American individuals are much more likely to be diagnosed below the age of 50 years, compared to White individuals. Having a first-degree relative with MM can also increase the risk of MM, especially among men and Black/African American individuals.2 Other risk factors include genetic alterations, environmental exposures, obesity, and alcohol consumption.1
As per the International Myeloma Working Group, the diagnostic criteria for MM are as follows:3
- Clonal bone marrow plasma cells of 10 percent or greater or biopsy-proven bony or extramedullary (outside the bone marrow) plasmacytoma (tumor formed by myeloma cells) and at least one of the following:
- Hypercalcemia (serum calcium >1mg/dL higher than the upper limit of normal or >11mg/dL)
- Renal insufficiency (creatinine clearance <40mL/minute or serum creatinine >2mg/dL)
- Anemia (hemoglobin >20g/L below the lower limit of normal or hemoglobin <100g/L)
- Bone lesions
- Clonal bone marrow plasma cells of 60 percent or greater
- Involved:uninvolved serum free light chain ratio of 100 or greater
- One or more focal lesions on magnetic resonance imaging (MRI)
- MM can lead to renal damage, platelet dysfunction, hyperviscosity (high blood viscosity), cytopenia (decrease in mature blood cells, eg, anemia, leukopenia, thrombocytopenia), and bone loss.1 Additional complications and symptoms include infection, bone pain, fatigue, venous thromboembolism, and peripheral neuropathy.1,2
Diagnosis and staging
In brief, the diagnostic process for MM includes a history and physical exam, blood tests, urine tests, bone marrow biopsy and aspiration, immunohistochemistry (IHC) and/or flow cytometry and fluorescence in situ hybridization (FISH), and imaging tests, typically 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). Blood tests can measure levels of red blood cell, white blood cells, platelets, antibodies, M protein, and free light chains. Urine tests can identify the levels of total protein, M protein, and light chains in the urine.4 Bone marrow aspiration and biopsy are necessary for determining the proportion of abnormal plasma cells,1 as samples collected from these procedures are used in IHC, flow cytometry, and FISH. IHC and flow cytometry identify myeloma cells in the bone marrow, and FISH detects chromosomal, or cytogenetic, abnormalities in myeloma cells, which aids in determining prognosis. FDG-PET/CT scans are used to show the location of the myeloma as well as any bone damage.4
The Revised International Staging System (R-ISS) and second revision of the ISS (R2-ISS) are often used to determine disease stage, which helps with risk stratification. R-ISS is divided into three stages:5
Stage I: ISS Stage I (serum beta-2 microglobulin <3.5mg/L, serum albumin ≥3.5 g/dL) and standard-risk cytogenetic abnormalities measured by interphase FISH.
Stage II: neither Stage I nor III
Stage III: ISS Stage III (serum beta-2 microglobulin ≥5.5mg/L) and high-risk cytogenetic abnormalities [ie, presence of del(17p) and/or translocation t(4;14) and/or translocation t(14;16)] measured by interphase FISH or serum lactate dehydrogenase (LDH) above the upper limit of normal
The R2-ISS assigns points to each risk factor based on their impact on overall survival. ISS Stage III is worth 1.5 points; ISS Stage II, presence of del(17p), serum LDH above the upper limit of normal, and t(4;14) are worth 1 point; and 1q gain/amplification is worth 0.5 points. Staging works as follows:6
Low-risk: score of 0; none of the risk factors listed above are present.
Low-intermediate–risk: score of 0.5 to 1
Intermediate-high–risk: score of 1.5 to 2.5
High-risk: score of 3 to 5
Treatment options vary based on patient characteristics, risk factors, and disease status (newly diagnosed or relapsed/refractory). The best way to understand whether a certain treatment option is right for you is to discuss it with your healthcare team.
Conclusion
MM is a rare and serious form of cancer that primarily affects older individuals. If you are diagnosed with MM, speak to your healthcare team about the treatment possibilities that fit best with your situation.
Sources
- Albagoush SA, Shumway C, Azevedo AM. Multiple myeloma. In: StatPearls. StatPearls Publishing; 2025. Updated 30 Jan 2023. Accessed 11 Apr 2025. https://www.ncbi.nlm.nih.gov/books/NBK534764/
- Padala SA, Barsouk A, Barsouk A, et al. Epidemiology, staging, and management of multiple myeloma. Med Sci (Basel). 2021;9(1):3.
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–e548.
- National Comprehensive Cancer Network. NCCN guidelines for patients: multiple myeloma, 2025. 2024. Accessed 11 Apr 2025. https://www.nccn.org/patients/guidelines/content/PDF/myeloma-patient.pdf
- Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863–2869.
- D’Agostino M, Cairns DA, Lahuerta JJ, et al. Second revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: a European Myeloma Network (EMN) report within the HARMONY Project. J Clin Oncol. 2022;40(29):3406–3418. Erratum in: J Clin Oncol. 2022;40(34):4032.




