By Emily Socolinsky
Coach Emily is the Owner and Head Coach of Fivex3 Training located in Baltimore, Maryland.
Bone density, an often overlooked element of women’s health, plays a critical role in our overall wellbeing and quality of life as we age. Unlike cardiovascular fitness or muscle tone, which tend to receive more attention in discussions of women’s health, bone strength quietly underpins everything from our ability to move freely to our resistance against fractures and long-term disability. The gradual and often silent decline of bone density, particularly in women, makes early education and screening, such as bone density dual-energy X-ray absorptiometry (DEXA) scans as early as 50 years of age, a vital part of preventative health care.
Bone mineral density (BMD) refers to the amount of bone mineral (hydroxyapatite) in bone tissue. It is measured using a DEXA scan, which evaluates the strength of bones and the likelihood of fractures. These scans yield two types of results: T-score and Z-score.
T-score compares your bone density to that of a healthy young adult. A T-score of –1.0 or above is normal. A score between –1.0 and –2.5 indicates osteopenia, a condition where BMD is below normal and may lead to osteoporosis. A score of –2.5 or lower signals osteoporosis, a disease characterized by fragile bones and an increased risk of fractures.
Z-score compares your bone density to the average of someone your age, sex, and weight. A Z-score significantly below average (<–2.0) may indicate that something other than aging is causing abnormal bone loss and should prompt further investigation.
For women, bone density is at its peak between the ages of 20 and 29 years. During this decade, the bones are the strongest and densest they will ever be. However, this window is fleeting.
Beginning around the age of 30 years, bone mass naturally starts to decline. The loss is slow and steady at first, often going unnoticed. By the time women are in their 40s, the rate of bone loss begins to accelerate, especially in the years leading up to menopause. Women may begin to show signs of osteopenia even without symptoms. Around the age of 50 years, women begin to enter menopause, and estrogen levels drop dramatically. Because estrogen is a key hormone in maintaining bone mass, this hormonal shift leads to a rapid decrease in bone density, increasing the risk for osteoporosis. For women in their 60s and beyond, without intervention, the risk of osteoporosis rises sharply. By this time, many women may experience fractures or learn that they have low bone mass only after an injury has occurred.
The Role of Menopause and Hormonal Changes
Estrogen plays a central role in bone remodeling, the process by which bones continually rebuild themselves. During menopause, the sharp decline in estrogen disrupts this balance, tipping the scale toward bone resorption (breakdown) rather than bone formation. This is why women are at a far greater risk of osteoporosis compared to men, especially after menopause.
Conditions like early menopause, surgical removal of ovaries, or amenorrhea (lack of menstruation due to underweight or high physical stress) can bring on early bone loss. Additionally, medications such as corticosteroids, certain thyroid treatments, and even some cancer therapies can reduce bone density.
Why Get a Bone Scan by 50 years of age?
Many health organizations recommend women begin routine DEXA scans at 65 years of age or earlier if risk factors are present. However, by this age, substantial bone loss may have already occurred. Detecting changes in bone density by 50 years of age allows women to take early action, including:
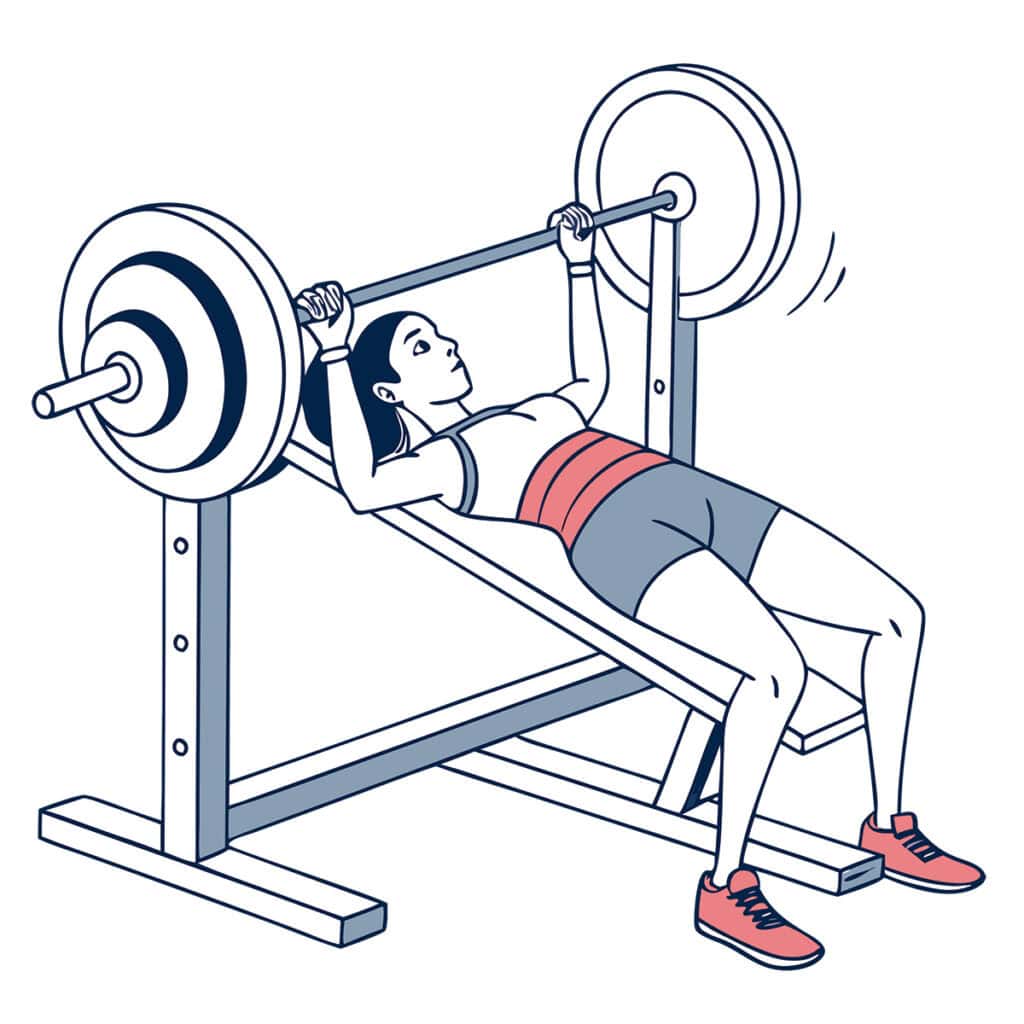
Implementing strength training. Resistance and weight-bearing exercises stimulate bone formation. Women who lift weights, especially heavy weights such as the compound barbell movements (squats, deadlifts, and presses), tend to maintain or even improve their bone density.
Supplementing wisely. Adequate intake of calcium and vitamin D is essential. Vitamin D helps the body absorb calcium and maintain healthy levels in the bloodstream. Women with vitamin D deficiency (<30ng/mL) are at greater risk of bone loss and fractures.
Addressing lifestyle risks. Smoking, excessive alcohol consumption, and very low bodyweight all increase the risk of osteopenia and osteoporosis. Identifying these factors early can allow for lifestyle interventions that preserve bone mass.
Monitoring medication impact. Some medications may affect bone density. Early scans can help track bone loss in women undergoing treatment for other conditions.
By the age of 50 years, most women are entering perimenopause or are already in menopause. This period is critical for assessing health risks, and adding a bone scan to routine checkups can uncover issues before a fracture occurs. It should be viewed as essential as mammograms or colonoscopies.
Real-World Evidence: Case Studies in Strength
Below are real-world case studies of five women between the ages of 50 and 75 years and the analysis of their bone scans during the time they implemented strength training into their lifestyle.
All five women had a DEXA scan, which is calculated as bone mineral content or mass divided by the projected area of a bone in a 2D image. These scans measured two-dimensional spaces, areal BMD (aBMD). An areal unit has no mass because area is a two-dimensional measurement of surface. It is calculated as cm² or m². Density, by definition, is mass per unit volume. Therefore, an areal unit, lacking mass, cannot have density.
In regards to aBMD, the focus is on mass per unit area, such as grams per square centimeter (g/cm²). This differs from volumetric BMD (vBMD), which is mass per unit volume (eg, g/cm3). While vBMD, obtained from 3D imaging techniques like micro-computed tomography (microCT), is a true measure of density, a DEXA scan which measures a two-dimensional space (aBMD), is an extremely valuable indicator of bone health and fracture risk even if it is not a true measure of density.
Case study 1: MS, a 75-year-old postmenopausal woman. MS has been training at Fivex3 since December 2019. Due to the COVID-19 pandemic, there was a 2.5-month period from mid-March to the end of May 2020 when she was unable to train due to the gym closure. MS resumed training in June 2020. She is a 75-year-old postmenopausal woman who underwent a BMD scan in 2023 that revealed ongoing concerns regarding her skeletal health. The scan indicated a diagnosis of osteoporosis in the femoral neck and osteopenia in the lumbar spine, along with moderate-to-high fracture risk over the next decade. Her previous scan was in 2021, and she is currently taking ibandronate, a prescription medication used to treat and prevent osteoporosis in postmenopausal women.
The World Health Organization (WHO) defines osteoporosis as a BMD T-score of –2.5 or lower. MS’s scan results confirmed this diagnosis in both hips, with a T-score of –2.5 in the left femoral neck and a T-score of –2.8 in the right femoral neck. These scores place her firmly within the osteoporotic range and are clinically significant because the femoral neck is a common site for debilitating hip fractures in older adults. Her lumbar spine presented a T-score of –1.7, which is categorized as osteopenia, a precursor to osteoporosis that also carries a notable risk for fracture, particularly in the setting of aging and hormonal changes.
The accompanying Z-scores (left hip: –0.91; right hip: –0.85; spine: 0.08) offer a comparison to age-matched peers. These values suggest that while her bone density was slightly below average in the hips, her lumbar spine BMD iwa essentially average for someone her age.
One of the more encouraging aspects of the 2023 report is the positive trend in bone density compared to her 2021 scan (during which she was training consistently three times per week):
- Left hip: +2.9 percent increase in BMD
- Right hip: +6.9 percent increase
- Lumbar spine: +6.2 percent increase
These gains suggest mild but meaningful improvements, possibly due to lifestyle changes, residual effects of previous medications, or increased calcium/vitamin D intake. However, these improvements, while statistically notable, do not reverse the underlying diagnosis. MS still qualifies as osteoporotic in both hips and remains at high fracture risk. But while she may qualify as osteoporotic in her hips, I would like to see a newer scan in 2025. If there was an increase in both hips and her lumbar spine between 2021 and 2023, I imagine there would be another increase in BMD between 2023 and 2025/2026.
Case study 2: HP, a 59-year-old postmenopausal woman. HP is a 59-year-old woman undergoing treatment for bone health and has had several BMD scans over the years, providing a valuable longitudinal dataset for understanding her skeletal health trajectory. She has been taking prednisone, a corticosteroid, for about 15 years. Corticosteroids are well known for their catabolic effects, particularly in reducing bone mineral density. HP was diagnosed with osteoporosis three years ago.
Her data spans from 2010 (age: 43 years) to 2024 (age: 58 years) and includes measurements taken before and after notable clinical interventions or medication usage. In 2010, HP started taking medication for bone density. HP joined a gym in 2007 and has been very active during the years between 2007 and 2023. Prior to October 2023, her fitness routine included spinning, body pump, and boot camp-style workouts 4 to 5 times per week.
Her first scan was in 2010 and at this time, HP’s BMD at the anteroposterior (AP) spine was 0.925g/cm², corresponding to a T-score of –1.1, which falls into the osteopenia range. By 2012, there was a modest increase to 0.940g/cm² (T-score: –1.0), an improvement of 1.7 percent. This gain, though small, indicated relative skeletal stability during this early period. In 2010, HP’s left hip BMD was 0.920g/cm² (T-score: –0.2), considered within the normal range. By 2012, the value increased slightly to 0.947g/cm² (T-score: 0.0), a 2.9-percent gain, indicating healthy bone remodeling and density.
However, there was an 11-year interval between her scan in October of 2012 and her scan in June of 2023, which saw a steep and concerning decline in spine BMD to 0.750g/cm², a loss of approximately 18.9 percent from baseline and over 20 percent compared to the 2012 level. The corresponding T-score dropped to –2.7, bordering on the threshold of osteoporosis. In addition to her decline in the spine, from 2012 to 2023, her BMD at the hip declined by approximately 13.9 percent, reaching 0.792g/cm² (T-score: –1.2), signaling a move into osteopenia territory. Although the decline was less dramatic than at the spine, it still represented a significant long-term reduction in bone strength and density.
What changed during this time to cause such a dramatic decline? During this time period, HP had stopped taking her bone density medication due to gastrointestinal complications and had also started hormone replacement therapy, as she was going through menopause. The decline in her BMD was almost certainly due to her stopping her bone density medication and the onset of menopause, as well as her lack of weight-bearing exercise. Despite HP’s active lifestyle, it is most certainly possible that the nature of her exercise—while cardiovascularly beneficial—did not sufficiently stimulate bone remodeling in a way that targeted the areas most at risk for osteoporotic fractures (eg, spine, hips). This underscores a key difference between general fitness and targeted resistance training in terms of bone health.
In October 2023, HP quit the gym she had been going to since 2007 and joined Fivex3 Training. She began a dedicated strength training program which involved the compound lifts—squats, bench press, deadlift, and overhead press. This meant no more boot camp classes, spinning, or body pump classes. One year later, in October 2024, she had her fourth DEXA scan, and a notable and encouraging shift occurred between June 2023 (4 months before joining Fivex3) and October 2024, with her BMD increasing in the AP spine from 0.750 to 0.805g/cm²—a 7.2-percent gain. The T-score improved to –2.2, pulling it back into the osteopenic range.
Most significantly, this gain exceeds the least significant change (LSC) threshold of 0.022g/cm², which means the improvement is statistically significant and likely reflects a true biological response rather than measurement variability. This positive trend strongly indicates that HP’s treatment—possibly pharmacologic (eg, bisphosphonates, anabolic agents) or lifestyle-based (eg, her new strength training program)—has been effective. In other words, the strength training program was working!
Her BMD at the hip remained relatively stable at 0.789 g/cm²—a slight decrease of just 0.4 percent, which is well below the LSC of 0.027g/cm². This minimal change suggests a plateau in bone loss at the hip, possibly reflecting the stabilizing effects of treatment, although not yet strong enough to induce a reversal as observed in the spine.
In conclusion, the AP spine, which was the most critical area of concern due to the dramatic loss between 2012 and 2023, showed a statistically significant and clinically meaningful improvement in the last year. This reversal implies effective recent intervention (like beginning a strength training program). In the hip, the decline was less severe compared to the spine, and while no significant improvement has occurred yet, the recent stabilization is a positive sign that the treatment may be beginning to halt further degradation.
As HP noted when we discussed her most recent scan, “I am physically stronger and have greater endurance. I also feel like I am psychologically stronger as I am taking charge of my health and am combating aging and a health condition that requires chronic steroid use. Getting yet another diagnosis [of osteoporosis] really weighed on me and after a short period of being upset, I set out to put in the work required to at least maintain the bone density that I have. So far it’s working!!”
Case study 3: ER, a 70-year-old postmenopausal woman. ER’s bone health trajectory from 2018 to 2024 offers an informative and nuanced picture of skeletal aging and resilience. The analysis focuses on two clinically significant regions: the AP spine (L1–L4) and the left total hip. Notably, ER did not use osteoporosis medications during this timeframe, allowing for an unfiltered view of natural or lifestyle-mediated changes in BMD. The data reveals divergent trends between the spine and hip, warranting a targeted interpretation of her results.
ER started taking CrossFit classes in 2018/2019 but then stopped attending those classes in 2020 due to the COVID-19 pandemic. During this time, she also underwent meniscus surgery on her left knee due to an injury and was doing physical therapy until October 2020.
In November 2020, she began strength training at Fivex3 Training and has been training there three days per week for the past 4.5 years. We started very slowly, being very conservative with the knee. In July 2023, she had a second meniscus surgery on the right knee. Before her second surgery, she was still training but began having more and more difficulty with her right knee. She followed up her surgery with physical therapy for three months, from July to September, and returned to Fivex3 Training in October 2023.
The AP spine has demonstrated a favorable trajectory in BMD, progressing from a baseline of 0.739g/cm² in 2018 to 0.797g/cm² in 2024. This 7.8-percent increase surpasses the region’s LSC threshold of 0.022g/cm², confirming the gain is statistically significant and not merely a reflection of measurement variability. More importantly, the associated T-score improved from –2.8 to –2.3, remaining within the osteopenic range but moving toward normal bone density.
This positive shift in spinal BMD is clinically meaningful. It reverses a prior period of decline, with the lowest recorded spine BMD occurring in 2022. The rebound since then not only reflects bone recovery but also suggests potential stabilization. Since no pharmacologic treatments were used, this improvement likely stems from lifestyle interventions, such as weight-bearing exercise (ie, squats, bench, overhead press, and deadlift) and nutritional intake (calcium and vitamin D).
The left total hip tells a more concerning story. From a baseline BMD of 0.786g/cm² in 2018, there was a net loss of 8.7 percent, culminating in a BMD of 0.718g/cm² in 2024. This reduction was accompanied by a T-score decline from –1.3 to –1.8, remaining within the osteopenic range but approaching the threshold for osteoporosis. While the decline is clinically significant, recent data provides a glimmer of cautious optimism: between 2022 and 2024, there was a modest BMD increase of 0.019g/cm² (+2.7%).
The bone loss in the left hip is not too surprising, as it was the left knee that she had injured in 2019 and had meniscus surgery on prior to beginning her strength program at Fivex3 Training. Despite this, the slowed rate of decline suggests a potential stabilization in hip BMD. As with the spine, the absence of pharmacological intervention points to nonmedication-related benefits, although the hip appears to be more resistant to recovery. This could reflect differences in mechanical loading or regional sensitivity to systemic changes (ie, her knee surgery).
ER’s six-year bone health experience reflects both vulnerability and resilience. Her spine has demonstrated a meaningful and statistically significant improvement in BMD, offering evidence of positive change and effective skeletal maintenance without medication. Conversely, her hip has undergone a moderate decline, with only recent signs of possible stabilization.
Case study 4: LH, a 60-year-old postmenopausal woman. Between 2021 and 2025, LH underwent three DEXA scans that tracked her progression and partial recovery of BMD during a medically complex period. Her skeletal health shifted from osteopenia to osteoporosis and then back toward osteopenia, reflecting the combined impact of trauma, systemic illness, pharmacologic therapy, and lifestyle modifications, including structured resistance training. LH had her first DEXA scan in February 2021, prompted by family history concerns. Her initial DEXA scan revealed osteopenia at multiple skeletal sites:
- Lumbar spine: BMD: 0.874g/cm²; T-score: –1.6; Z-score: –0.4 (osteopenia)
- Left hip (total): BMD: 0.852g/cm²; T-score: –0.7; Z-score: 0.0 (normal)
- Left femoral neck: BMD: 0.671g/cm²; T-score: –1.6; Z-score: -0.5 (osteopenia)
A one-inch height loss (from 5’6” to 5’5”) was documented, possibly due to early spinal compression or postural shifts. At this stage, the bone loss was mild and did not yet meet the criteria for an osteoporosis diagnosis. Two years later in March 2023, she had a follow-up scan, and unfortunately, it was not what she expected, as it marked significant deterioration:
- Lumbar spine: BMD: 0.762g/cm²; T-score: –2.6; Z-score: –1.3 (osteoporosis)
- Left hip (total): BMD: 0.791g/cm²; T-score: –1.2; Z-score: –0.4 (osteopenia)
- Left femoral neck: BMD: 0.610g/cm²; T-score: –2.2; Z-score: –0.9 (osteoporosis)
However, prior to this 2023 scan, in November 2022, LH suffered three pelvic fractures in a high-speed bicycle accident. This traumatic event most likely led to decreased mobility and increased systemic stress, both risk factors for rapid bone loss.
To add more fuel to the fire, in February 2024, LH had a computed tomography (CT) scan, followed by a positron emission tomography (PET) scan in March, as well as a bronchoscopy (a medical procedure where a doctor uses a thin, flexible tube called a bronchoscope to examine the airways and lungs). After this procedure, she was diagnosed with lung cancer and had a lobectomy (lobe removal) of the upper left lung and a wedgectomy (wedge resection) of the lower left lung. She began chemotherapy in June 2024 and completed her last treatment in August. LH began immunotherapy in September 2024.
In June 2025, she had her third bone scan. This scan was much more promising than her 2023 scan. Despite a lung cancer diagnosis and intensive treatment, the 2025 DEXA scan showed modest BMD improvement across all measured sites. Notably, the lumbar spine T-score improved enough to move out of the osteoporotic range, indicating successful skeletal stabilization. This is especially remarkable given the bone-depleting effects of chemotherapy and systemic illness. Her scores were as follows:
- Lumbar spine: BMD: 0.805g/cm²; T-score: –2.2; Z-score: –0.7 (osteopenia; a 5.7% increase)
- Left hip (total): BMD: 0.824g/cm²; T-score: –1.0; Z-score 0.0 (osteopenia, getting close to being normal again; a 4.1% increase)
- Left femoral neck: BMD: 0.625g/cm²; T-score: –2.0; Z-score 0.7 (osteopenia, a 2.5% increase)
What could have made the difference between her 2023 scan of osteoporosis and her 2025 scan that put her back in the osteopenia range? She began a once-per-year infusion of zoledronic acid, a potent bisphosphonate that reduces bone turnover and fracture risk. She also began a consistent weekly strength training program in June 2024 at Fivex3 Training.
On May 28, 2024, LH emailed Fivex3 Training. “Hello. I am 59 and have been an athlete most of my life. Recently diagnosed with both osteoporosis and cancer. I am looking for a strength program to maximize my muscles and do my best to bulk up.” On June 10, 2024, one week after her first chemotherapy treatment, LH began a structured weekly barbell strength training program, incorporating squats, bench presses, overhead presses, and deadlifts. She continued this regimen throughout chemotherapy (June–August) and immunotherapy (September–July) and remains consistent with it today.
This type of high-intensity, compound movement training is one of the most effective nonpharmacologic strategies for stimulating osteogenesis, particularly in postmenopausal women. Its timing—coinciding with BMD improvement despite systemic stress—strongly suggests a positive synergistic effect alongside zoledronic acid in promoting skeletal resilience.
LH’s case is a compelling example of how multimodal intervention—pharmacologic, rehabilitative, and behavioral—can improve bone health even in the context of trauma and systemic disease. Her BMD gains, while modest, are clinically meaningful and encouraging. With continued engagement in treatment and lifestyle management, LH’s skeletal health can remain stable—or even improve—despite age-related and oncologic challenges.
Case study 5: ES, a 50-year-old menopausal woman. ES is a 50-year-old woman whose bone health reflects the long-term benefits of an active lifestyle and strength training. Her first and recent DEXA scan reveals a skeletal profile that is not only well-preserved but also unusually robust for her age. This case provides a unique opportunity to explore the intersection of lifestyle, physiology, and diagnostic interpretation in the context of bone health.
ES has maintained a physically active lifestyle for nearly her entire life. From early childhood until 35 years of age, she participated in dance, first at a competitive level and later recreationally. At 35 years of age, she transitioned into strength training, engaging in consistent, progressive resistance exercise for the past 15 years. Her regimen includes fundamental compound movements, such as squats, deadlifts, bench presses, and overhead presses—exercises known to exert high mechanical loads on the skeleton, especially on weight-bearing bones such as the spine and hips. This longstanding commitment to physically demanding activity is a key contextual factor for interpreting her DEXA results.
ES’s DEXA scan of the lumbar spine (L1–L4) showed individual BMD values ranging from 1.341 to 1.440g/cm², with an average of 1.366g/cm². These values translate to T-scores between +3.0 and +3.6, and Z-scores between +3.6 and +4.3. According to the WHO, a normal T-score lies between –1.0 and +1.0. Her scores far exceed this range, indicating a bone density more than three standard deviations above the young adult mean—an extraordinarily rare outcome.
While high BMD is typically advantageous and suggests superior skeletal strength, the magnitude of ES’s scores is unusual. Z-scores greater than +2.0 are also considered elevated when compared to age-matched norms, which may prompt further evaluation. Although these results raise questions about potential underlying factors, they must be interpreted in the broader context of her health and lifestyle.
In contrast to the exceptionally high spinal scores, ES’s femoral neck and total hip BMD results fall within the high-to-normal range. Her femoral neck BMD measured 1.029g/cm² with a T-score of +1.6, while her total hip BMD was 1.158g/cm² with a T-score of +1.8. Z-scores for these regions were +2.4 and +2.2, respectively. These values confirm that ES’s skeletal robustness is not isolated to the spine and reflects consistent adaptation across multiple anatomical sites due to mechanical loading and muscular development.
To complement BMD, her lumbar spine DEXA image was also analyzed using a trabecular bone score (TBS), which evaluates bone microarchitecture. Her TBS was 1.552, well above the threshold of 1.31 that indicates healthy trabecular structure. This finding affirms the quality and organization of her bone tissue, supporting the interpretation that her high BMD reflects not just density but also structural integrity.
ES’s comprehensive scan results suggest an extremely low risk of osteoporotic fracture. Her elevated BMD, favorable TBS, and absence of any history of fragility fractures all contributes to a skeletal profile that is resilient and structurally sound. The FRAX tool, used to estimate 10-year fracture probability, was deemed unnecessary due to her high T-scores, further underscoring her low risk.
ES’s case exemplifies how a lifetime of physical activity—particularly involving weight-bearing and resistance training—can yield extraordinary benefits for skeletal health. Her results not only highlight the potential of lifestyle interventions in preserving bone strength but also serve as a reminder to approach outlier values with careful, contextual interpretation. ES represents an optimal case of midlife bone health. Her DEXA scan results reflect both a high-density and high-quality skeletal structure, positioning her at a minimal risk for fracture and providing a powerful model for healthy aging.
Conclusion: Strong Bones, Stronger Women
Women no longer need to accept declining bone density as a part of aging or suffer silently through the consequences. We are in an era where information is accessible, preventative care is encouraged, and personal agency is celebrated.
Talking about menopause, osteopenia, and osteoporosis openly—as Gen X women are doing now—allows us to rewrite the narrative for ourselves and future generations. A DEXA scan at 50 years of age is not just a diagnostic test; it is a declaration that you matter, that your health is worth tracking, and that you are not powerless in the face of aging. Strong bones are not built in a day, but the decision to start protecting them can be made today.




